What Is HELLP Syndrome?
HELLP syndrome is a rare but potentially dangerous condition that affects pregnant women. It tends to occur after childbirth or later in the pregnancy, and the condition is closely associated with preeclampsia. It was first named in 1982 by the doctor who described the condition, Dr. Louis Weinstein.
The name HELLP is an acronym taken from the main characteristics of the condition. These are hemolysis, elevated liver enzymes, and low platelet levels. Treatment and management for this condition are available, but it should be found as soon as possible because the condition is potentially dangerous to both the mother and the child.

1. Etiology
The cause of HELLP syndrome is unknown; some consider it a form of preeclampsia, while others propose that it is a different entity.
Preeclampsia is a disorder that occurs after 20 weeks’ gestation until six weeks postpartum. Clinically, it presents as high blood pressure (according to specific BP criteria) and proteinuria or abnormal quantities of protein in the urine. This may or may not be associated with edema or the swelling of the upper and lower extremities.
The theory that HELLP syndrome is a variant of preeclampsia, suggests that they may have a common etiology. In preeclampsia, structural reorganization (remodeling) of the placental blood vessels results in inadequate blood flow to the placental tissues. Consequently, the placenta releases several growth factors that cause placental dysfunction and damage the cells that line the blood vessels (endothelial cells) of multiple organs. This cascade of events can result in maternal hypertension, proteinuria (due to kidney damage), and increased activation of the coagulation cascade (i.e. platelet activation and aggregation).

2. Risk Factors
Although the cause of HELLP syndrome remains unknown, there are several risk factors associated with the condition. One of them is multiparity or giving birth two or more times. Other risk factors include maternal age over thirty-four, white race or European descent, and a history of poor pregnancy outcome.
Curiously, the risk factors for HELLP syndrome can be different from those associated with preeclampsia. For example, the condition in a woman of never having given birth (nulliparity) is a risk factor for preeclampsia.
3. Hemolysis
Our blood cells are essential because they transport and supply the rest of the body with oxygen from our lungs. Normal red blood cells have a life span of approximately 120 days. When our blood cells come to the end of their lives, they are broken down by our bodies in a process known as hemolysis, in order to recycle some of their components. In HELLP syndrome, red blood cells are broken down too soon.
In this condition, the lining of many blood vessels (endothelium) is damaged; thus, certain molecules within the wall of the vessels become exposed and cause the activation of the coagulation cascade. Once activated, it causes platelet adhesion onto the damaged endothelium. Importantly, as red blood cells pass through tiny blood vessels(capillaries), these platelet-fibrin deposits may cause their fragmentation. This process of hemolysis decreases the general mass of red blood cells in the body, causing microangiopathic anemia (anemia that is caused by a condition that affects tiny blood vessels).
In patients with HELLP syndrome, a peripheral smear might be performed to provide information about the shape (and number) of blood cells in the body. This test might reveal schistocytes or fragmented red blood cells that can be irregular and take on different shapes.

4. Low platelet count
When there is a loss of continuity on the lining of one of our blood vessels, platelets are the main cells in charge of the first step of hemostasis, or the process of stopping the bleeding, by forming a primary plug on the affected site.
As mentioned above, the damaged and activated endothelium in HELLP syndrome can lead to the activation of the coagulation cascade. As a consequence, there can be increased consumption of platelets as they adhere to this endothelium. Thus, patients with HELLP syndrome can exhibit thrombocytopenia, which is characterized by abnormally low levels of platelets (thrombocytes) in their blood.

5. Elevated liver enzymes
The endothelial disruption that occurs in HELLP syndrome can also affect the blood vessels in the liver. As mentioned before, endothelial insult leads to platelet activation and fibrin deposition, which can ultimately lead to the obstruction of blood flow through hepatic sinusoids (blood vessels). When the cells of the liver, especially those localized around the portal venules, receive inadequate perfusion they may eventually undergo a process of cellular death known as necrosis (periportal necrosis) that can result in liver failure. Furthermore, in severe cases, liver damage can be extensive (i.e. intrahepatic hemorrhage, subcapsular hematoma, hepatic rupture).
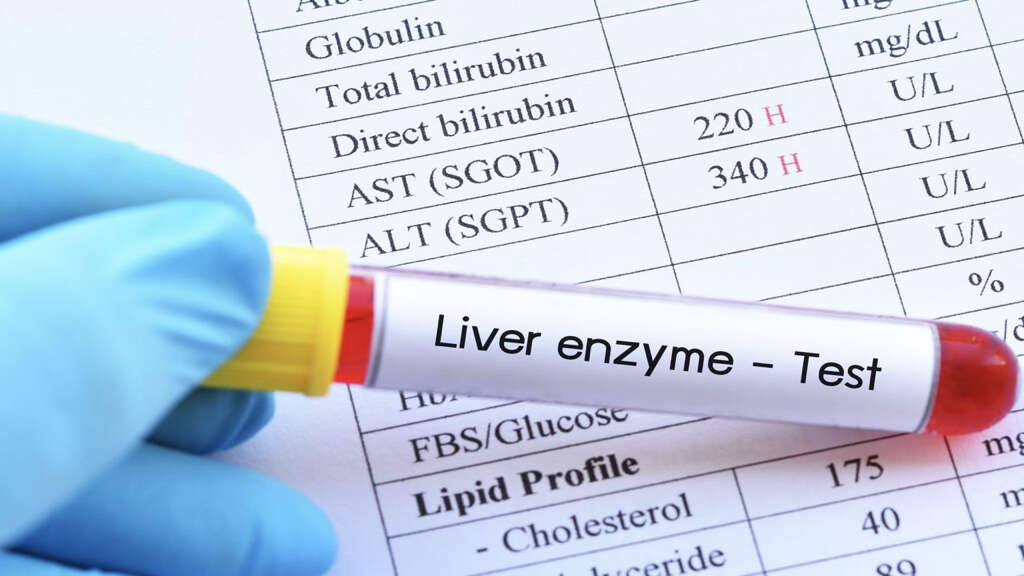
Importantly, liver damage can be detected through the elevation of certain liver enzymes known as transaminases: alanine transaminase (ALT) and aspartate transaminase (AST). However, transaminase elevation is not specific for HELLP syndrome.

6. Diagnosis
Getting a correct diagnosis for HELLP can be difficult. The condition may cause several signs and symptoms, but their occurrence varies greatly from patient to patient. Due to the variable nature of the clinical presentation of HELLP syndrome, the diagnosis is usually delayed for approximately 8 days. Patients with this disease are initially misdiagnosed with other conditions, such as viral hepatitis, peptic ulcer disease, hyperemesis gravidarum, and other causes of thrombocytopenia (low platelet levels).
The physician may start to suspect HELLP syndrome, especially in pregnant women, through a series of vague complaints such as nausea, vomiting, malaise, abdominal pain (upper abdomen), or difficulty breathing (i.e. pulmonary edema). Additionally, the physician will perform a physical examination of the patient which may reveal other nonspecific findings such as fluid buildup in the upper and lower extremities (edema), signs of dehydration, tenderness in the right upper abdomen, and jaundice. In HELLP syndrome, vital signs may also be altered, including blood pressure (hypertension), heart rate (tachycardia), and respiratory rate (tachypnea).

7. Abdominal pain
As mentioned, HELLP syndrome can affect the liver, causing its enlargement. As a result, women with HELLP syndrome will often feel tenderness or pain when touching the upper-right side of their abdomen, which is where the liver is located.
Also, patients with HELLP syndrome may experience pain in the middle of the upper-abdomen, also known as epigastric pain.

8. Dyspnea
In general, there are many causes of dyspnea, which is a medical term for shortness of breath. Dyspnea can be a symptom of pulmonary edema; however, note that it is not exclusive of this condition. Similarly, pulmonary edema can be caused by several other pathological processes.
The alveoli are tiny air sacs in the lungs that constitute the functional unit of the organ, where gas exchange takes place. Pulmonary edema is caused by the accumulation of fluid in the supporting framework of the alveoli (interstitium) and the alveolar spaces of the lung. This edema, if severe, can be life-threatening because it impairs the exchange of gases by decreasing the diffusion of carbon dioxide and oxygen. Pulmonary edema is rare during pregnancy; however, it can occur as a complication of preeclampsia and HELLP syndrome.

9. Workup: diagnostic tests
Once physicians have identified possible signs and symptoms of HELLP syndrome in a patient, they must run a series of tests to corroborate the diagnosis. A complete blood count (CBC) in a patient with this condition might report anemia and a normal or low hematocrit (the volume percentage of red blood cells in the blood) as a result of hemolysis. Furthermore, thrombocytopenia or an abnormally low platelet count can also be reported. The doctor will also order a peripheral smear if hemolysis is suspected (i.e. schistocytes). As mentioned, to evaluate possible liver involvement, liver function tests can be ordered. Liver substances or enzymes that may be abnormally elevated in HELLP syndrome include transaminases (ALT and AST), lactate dehydrogenase (LDH), and total bilirubin.
In a patient with HELLP syndrome, many aspects need to be monitored, including kidney function. If kidney function is impaired, a complete metabolic panel can report elevated blood urea nitrogen (BUN)/creatinine and urine tests can report proteinuria or the presence of abnormal quantities of protein in the urine. Importantly, note that many of the alterations reported by these tests may also be present as a result of other pathologic processes.

10. Management and Treatment
The first step in the management of HELLP syndrome is the immediate identification of the diagnosis through physical examination, history, and laboratory findings. While the patient is being transferred or once already in the emergency department, immediate stabilization of the condition is of great importance. Stabilization of the patient might include seizure prevention, blood pressure control, and transfusion of blood or blood products.
Certain medications for seizure prevention and blood pressure management may be warranted at this time. Once the condition is stabilized, close observation of the patient begins in a monitored labor unit under obstetric care. If HELLP syndrome is diagnosed close to 34 weeks’ pregnancy, vaginal delivery or C-section can be indicated.












